Varicose veins (varicose veins) are a disease that is accompanied by an increase in length, the formation of serpentine pathological convolutions of the veins, irreversible sac-shaped enlargements of their lumen and valve insufficiency. The organs of the lower pelvis are involved in the varicose vein process. The mechanisms of development of the disease are different. Doctors count the perineal region, external and internal genitals as atypical locations.
General information on pathology
The flow of blood through the veins is such that, under physiological conditions, conditions are created for the development of stagnation and blood outflow.
Varicose veins of the vulva (VV) - vasodilation of the external genitalia. The disease manifests itself in women suffering from varicose veins of the pelvis and legs, as well as in pregnant women. Pelvic varicose veins affect the perineum and vulva in 30% of cases.
The start of treatment for the disease is delayed due to its location in an intimate place. Women are shy. In some cases, patients feel no pain or discomfort. But varicose veins of the labia during pregnancy, and not only when carrying a fetus, run with complications: clogging of the veins with a thrombus (thromboembolism), disorders of sexual sensitivity, pain in the perineum, psycho-emotional problems and family conflicts.
The mechanisms by which pelvic vasculature congestion occurs are not fully disclosed. The cause of the primary form of the disease is called malfunction of the valves of the gonadal (ovarian) veins. This provokes a backflow of blood and increases the pressure in the venous nodes of the lower pelvis. Valve insufficiency can be acquired or congenital. It gets worse with age or with pregnancy.
The secondary form of VVV of the pelvic organs is associated with gynecological pathologies: endometriosis, tumors of the pelvic organs.
Diagnosing the disease is difficult because there are no specific symptoms of its course. It is based on the results of ultrasound (ultrasound).
To distinguish the primary and secondary pathology, the Valsalva test is used during the sonographic examination. If there is a secondary cause of pelvic varicose veins, it is negative.
Varicose veins of the labia with VBT
To make a diagnosis of varicose veins of the labia, a medical examination is required. The symptoms of the disease are as follows:
- Varicose veins on the genitals;
- Pain in the external genital area;
- a feeling of heaviness and burning in the perineum;
- Swelling of the perineum at the end of the day.
Chronic pelvic pain occurs less often (in 30% of cases).
After the diagnosis is made, a study is carried out to determine the degree of complexity of the pathological process and prescribe appropriate treatment. Various events take place:
- Examination of the veins of the perineum and legs by ultrasonic angioscanning - USAS;
- Performing ultrasound of the pelvic vessels, including the vaginal, uterine, parametric, ovarian, iliac, inferior vena cava, and renal veins;
- Depending on the indication, multispiral computed tomography (MSCT), selective ovarkography and pelvic phlebography (SOFT) are performed.
Doctors call a characteristic feature of varicose veins on the labia in VBT that the disease progresses steadily and is associated with the transformation of the pelvic veins.
Treatment of varicose veins of the vulva with varicose veins of the lower pelvis
IV treatment is prescribed based on the symptoms and diagnostic results.
In complex drug therapy for the treatment of systemic chronic venous pathology, nonsteroidal anti-inflammatory drugs and phlebotropic drugs are prescribed.
Prescribe antiplatelet drug pharmacotherapy, intrapelvic blockade with antihypoxants, ultrasound physiotherapy, therapeutic exercises. Antioxidants and enterobiotics are added to the therapy.
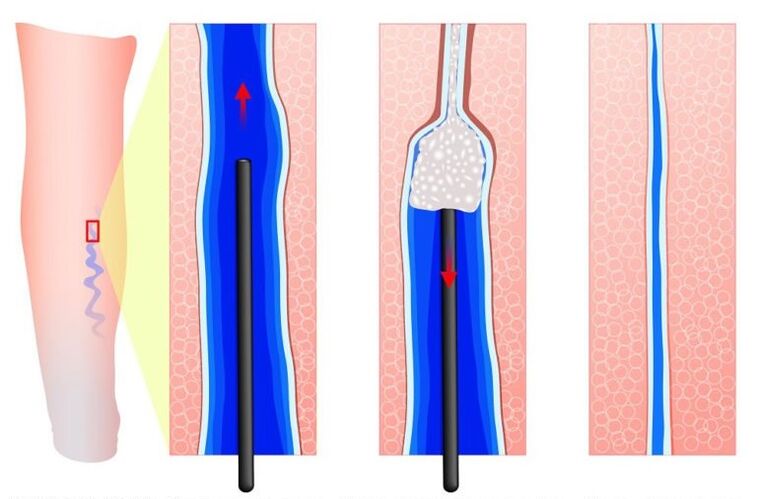
Depending on the indication, phlebosclerosing treatment is carried out - sclerotherapy. The vessel is "sealed" with medication and a laser. It stops working. The procedure does not use any special anesthetic methods. It is performed on an outpatient basis and has a cosmetic effect.
If pelvic vein abundance, expansion, and backflow of blood through the gonadal (ovarian) veins, surgical operation to remove the veins is indicated. If there is an enlarged varicose vein in the labia minora, this is removed.
Varicose veins of the vulva during pregnancy
Pregnancy is the most common risk factor leading to the occurrence of VVV. A significant and sustained increase in progesterone levels in the early stages of pregnancy reduces venous tone and aggravates circulatory disorders. In addition, VBT, which affects the perineum and vulva, is associated with the compression of the large veins of the retroperitoneal region (pelvic veins and inferior vena cava) by the pregnant uterus.

Doctors recommend compression stockings during pregnancy.
Often, varicose veins of the vulva occur on both sides. Signs of illness:
- a pronounced increase in vulvar veins over a period of 18-24 weeks during the first pregnancy, from 12 weeks with a repeated pregnancy;
- discomfort in the groin;
- pulling, aching, dull pains in the pelvic area;
- Painful intercourse;
- Itching of the vulva;
- Swelling of the genitals and perineum.
Signs of pathology progress as pregnancy progresses. In addition to the enlargement of the varicose veins, their compaction is determined by the third trimester. A characteristic symptom of IV is the combination with inguinal varicose veins during pregnancy or varicose veins in the legs.
The instrumental examination of varicose veins of the labia in pregnant women is limited to their sonography and sonography of the legs, since painful changes in the venous bed are regressed in the postpartum phase.
In most cases (around 80%), symptoms of varicose veins during pregnancy begin to decrease from the first days of birth and are minimized 2-8 months after the baby is born. There is no complete return of the diameter of the vessels to their original values.
In 4-8% of women, IV does not go away after childbirth and the disease progresses.
An interesting feature is the relationship between the end of breastfeeding or a decrease in breastfeeding volume and the rate of disappearance of varicose veins in the groin in women. A shortened breastfeeding period is accompanied by a decrease and disappearance of dilated veins and vice versa. This proves that varicose veins of the perineum are associated with a change in hormone levels during pregnancy.
Treatment of varicose veins of the perineum during pregnancy
The basis of therapy for varicose veins during pregnancy is phlebotropic treatment. In most fertile women, IV begins in II and III. Trimester. Diosmin preparations can be used during this time. The severity of the pathological symptoms is reduced by the micronized purified flavonoid fraction. Itching is relieved by zinc paste and H1 histamine receptor blockers.
Low molecular weight heparin in a prophylactic dose prevents venous thrombosis and pulmonary embolism (blockage of blood vessels).
As an option for compression treatment, tight-fitting elastic underwear with latex or gauze pillows is mandatory. It relieves the swelling of the labia and the feeling of heaviness. Special compression jersey for women with varicose veins on the vulva helps a lot.
If a complication develops, such as local thrombophlebitis, surgical treatment is required.
If a conglomerate of varicose veins is found on the genitals, the question of the nature of the delivery arises. With varicose veins of the vulva, natural birth is allowed. On the contrary, the risks of an operation during a caesarean section are higher than the onset of bleeding from painful vessels during childbirth. This rarely happens. But with varicose veins of the vagina, a caesarean section is often done.
Prevention of varicose veins of the labia
The main factor in the formation of varicose veins in the groin is the birth of the fetus. It is difficult to name preventive methods, considering that many therapeutic measures are limited during pregnancy. Some tips to follow:
- exclude physical and static stress;
- follow a diet;
- perform therapeutic exercises, during which movements accelerate the outflow of blood from the legs and lower pelvic organs;
- With a disorder in the work of veins, the presence of varicose veins before pregnancy, it is necessary to take phlebotropic drugs, wear compression underwear.
An effective method of prevention is considered to be an operation on the ovarian veins, an operation for other pathologies associated with varicose veins. This reduces the phenomenon of pelvic vein congestion and reduces the risk of varicose veins in the labia.
Varicose veins of the vulva are a common condition in women with varicose veins of the pelvis, legs, or during pregnancy.
In order to improve the quality of care for patients with chronic venous disease, it is important to recognize the disease and differentiate between the methods of diagnosis and treatment of the disease.




































